The Sargeant Health Center is bustling early on a Monday morning. I’ve been invited to put on scrubs and watch as Geoff Wilkes, MD, Assistant Professor of Ophthalmology, Medical College of Wisconsin, performs a cataract surgery. As I stand off to the side, the team diligently sets up the room, checks their notes, and prepares the tools and visuals necessary to perform surgery.
Susan, Dr. Wilkes’ first patient of the day, is back for her second surgery to remove the cataract from her left eye following the previous week’s removal of the cataract on her right.
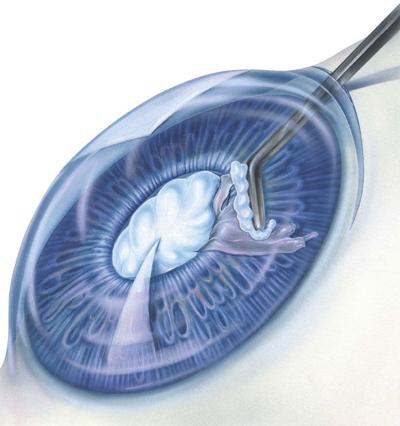
Promptly at 7:30 a.m., Susan is wheeled into the room, prepped, and the surgery begins. Dr. Wilkes gently explains each maneuver and step in the surgery. Less than 10 minutes later, the cataract has been removed and an intraocular lens has been implanted, allowing Susan to see much more clearly.
Insight Into Cataracts
The American Academy of Ophthalmology notes that cataracts affect more than 24.4 million people, and by age 75 more than half of the population will develop cataracts.
A cataract is when the lens of the eye loses its clarity (usually identified with any cloudiness, haziness or opacification in the lens), explains Dr. Wilkes. Though cataracts can develop for many reasons, the most common cause is the natural aging process.
“With age and increasing lens fiber density, the very regular arrangement of lens proteins breaks down and becomes less regular. This irregularity causes the lens to become less clear,” says Dr. Wilkes. “Other than aging, common causes of cataract development include use of corticosteroid medications, poorly controlled diabetes mellitus, eye trauma, intraocular inflammation — also known as uveitis — and numerous gene mutations.”
Jason N. Edmonds, M.D., Cataract, Cornea, and Refractive Surgeon at Milwaukee Eye Care, explains that the only solution for cataracts is surgery. During that process, the cloudy lens is removed and replaced with a lens implant. Dr. Edmonds notes that a surgery can either be done manually under a high-power operating microscope or via a laser assisted surgery wherein the surgeon programs a computer-guided laser to assist in some steps of the removal.
“The laser can also be used to correct astigmatism,” he adds. “The quick recovery after cataract surgery allows patients to resume many of their normal activities in the first 24 hours following surgery. In the first 12-24 hours, patients often experience blurry vision, light sensitivity and mild irritation. Some restrictions are placed on physical activity in the first week after surgery, but most patients can resume the majority of their day-to-day.”
“Recovery from cataract surgery is generally straightforward, but can vary depending on a person’s pre-existing medical conditions and the density of the cataract that they have removed,” Dr. Wilkes adds. “Most patients use prescription anti-inflammatory eye drops for a few weeks after surgery to help the eye to heal safely and avoid swelling that can inhibit good vision. For one week following cataract surgery, I ask patients to avoid vigorous exercise, heavy lifting and submerging their head underwater.”
Milwaukee Eye Care’s Cataract Surgeon and Glaucoma Specialist Nicholas J. Frame, M.D., adds that he diagnoses cataracts multiple times a day and performs anywhere from one to two dozen cataract surgeries each week.
“This has been pretty consistent,” he says. “However, as the population ages, this will continue to increase. We’ve noticed an increase in cataract surgeries when pandemic restrictions were lifted, as many patients delayed routine or non-urgent medical visits.”
Lens Replacement
Whether a patient is experiencing nearsightedness or farsightedness, Dr. Wilkes explains that the procedure is the same, the only difference being the prescription on the lenses implanted.
“We choose the power of the intraocular lens depending on the goals of the patient,” he explains. “When not wearing glasses, does the patient want to see best in the distance following surgery? See best at near? Or both? Does the patient want their astigmatism corrected with the intraocular lens placed at the time of surgery?”
Back in her room post-surgery, Susan explains to me that she’s worn glasses and contacts since she was young, and is ecstatic to leave the surgery not only without the cataracts, but without needing to use her glasses anymore — she won’t have to wear glasses at her son’s upcoming wedding, thanks to the lenses.
Later, Dr. Wilkes discusses cataract treatment. “While everyone will develop cataracts as they age — it’s commonly said that 80 percent of people will have visually significant cataracts by the age of 80 —patients shouldn’t feel an urgent need to have cataract surgery as soon as they hear it mentioned during an eye exam,” he says. “Cataracts often take many years to develop into something that is visually significant, and surgery is not indicated until a patient’s vision is affecting their quality of life and activities of daily living.
“The decision to move forward with cataract surgery should be informed by how a patient is functioning with their vision, not what an optometrist or ophthalmologist sees on examination,” Dr. Wilkes says.
Susan is squeamish around eyes, and had even written off the idea of LASIK due to her fears. But now that she’s cataract-free and has 20-20 vision, she highly encourages anyone who might have cataracts to take the plunge.
“You talk about other surgeries: back surgeries, knee replacement, hip replacement,” she says. “You have to go through rehab, and recovery takes a long while. THIS is the immediate gratification. That's my long PSA that people really shouldn’t wait.”
Patients tend to be incredibly happy not only with the quick surgery and short recovery, but the immediate results, Dr. Wilkes says.
“There are few things better than seeing patients in the clinic the day after surgery and hearing them describe seeing something for the first time in a long while, even though those things might be dust on their counters or wrinkles on their face,” Dr. Wilkes says. “Helping patients increase their quality of life by improving their vision never gets old.” MKE
LASIK: Is It For You?
My husband has considered LASIK for the ease of his job. I’ve considered it, simply so I can wake up and see without having to put in contacts or throw on my glasses.
No matter the reason, the procedure promises clear vision without the hassle of putting on lenses, and remains one the most common types of corneal-based refractive surgery, according to Jason N. Edmonds, M.D., an ophthalmologist specializing in cataract, cornea, and refractive surgery. The surgery utilizes lasers to reshape the cornea and adjust nearsightedness, farsightedness and astigmatism.
Though there are other forms of cornea based refractive surgery, LASIK, or laser-assisted in situ keratomileusis, is “one of the most common types of corneal based refractive surgery,” he says. The procedure uses lasers to reshape the cornea and adjust nearsightedness, farsightedness and astigmatism.
Similar to the immediate gratification of a cataract removal, Dr. Edmonds notes that recovery is quick, with patients typically able to resume normal activities within 24 hours post-surgery.
“Patients choose LASIK because it offers reduced dependence on glasses and contact lenses,” explains Dr. Edmonds. “In the appropriate patient, LASIK is safe, has a low risk of complications, allows rapid recovery, and a quick return to normal functioning.”
While many might be interested in ditching their glasses or contact lenses, not all patients are good candidates. Those with high vision correction needs, thin corneas or some form of eye disease may not be eligible, Dr. Edmonds says.
“It’s always important to have a thorough consultation and a detailed discussion of risks with a refractive surgeon before proceeding with surgery,” he notes.
Whether you’re considering LASIK or not, Dr. Edmonds offers some tips for healthy eye care: “For adults, the American Academy of Ophthalmology (AAO) recommends screening eye exams once in your 20s and twice in your 30s. Healthy adults with good vision should have a complete eye exam at age 40. Those with diabetes, high blood pressure, or a family history of eye disease shouldn’t wait until age 40 for a complete eye exam.
“If you’re age 65 or older, the AAO recommends a full eye exam every 1-2 years to check for signs of age-related eye disease such as cataracts, glaucoma, and macular degeneration,” he continues. “For children, the American Academy of Ophthalmology and the American Association for Pediatric Ophthalmology and Strabismus have developed specific screening guidelines to identify when a child may need a complete eye exam.”